By Tyler Norris and Benjamin F. Miller
Our nation faces layered social, economic, political, climate and health crises, including a crisis of mental health and addiction. Alongside hundreds of thousands of deaths from COVID-19, the growing problem of “deaths of despair” will increase due to underlying trauma, social disconnectedness, and profound economic fallout stemming from the pandemic. But even before COVID-19, these issues of despair were killing us. Change is possible, starting with pragmatic action in our communities.
To move beyond our collective pain to a place of healing, we must begin by addressing the mental, emotional, and spiritual well-being of the American people just as urgently as we put in place strategies for civic and economic renewal. Federal and state support are vital. But because we are a nation divided and federal action has been slow in coming, comprehensive action at the local and state level shows the greatest promise to save lives and promote widespread healing.
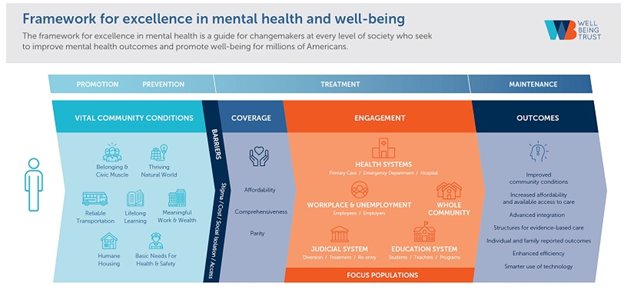
Measurably improving mental health and well-being will require us to tackle three areas at once: coverage, care delivery, and community conditions that promote health. There are concrete actions local leaders across a community — including health care institutions, nonprofits, schools, business, faith leaders and government — can take in each of these areas.
Pain in the Nation
Health is the foundation for all human achievement. Without it, we cannot reach our goals, accomplish meaningful tasks, or thrive. The science on what makes — and keeps — us healthy has matured, and we know a lot more than we used to about the factors far beyond health care that positively and negatively impact our physical and mental health and well-being.
Not too long ago, no one would have suggested the ZIP code where someone lives plays a greater role in how healthy they will be or how long they will live than their access to care or their genetics. Now we understand that place matters. We know that social, economic, and environmental factors — like the availability of social connections, jobs, and clean air to breathe — create the conditions for positive health and well-being. These factors differ greatly from place to place and shape disparities by race and ethnicity.
We also know better now than ever how critical our mental health is to our physical health and overall well-being. Yet still too often, mental health and addiction are treated separately from physical health, making it challenging for people to get timely access to quality mental health and addiction services.
Despite our understanding of these issues, our nation’s health continues to go in the wrong direction. Except for a very modest recent increase, life expectancy has been on the decline for the past few years. We are losing more people in the prime of their lives to deaths from preventable causes — drug overdose, suicide, and alcohol abuse — than ever before. In 2018 alone, 151,964 Americans died due to alcohol, drugs, or suicide.
This national death rate for what are often called deaths of despair was only slightly lower than the year before, despite progress in reducing some types of opioid overdose, according to a study by Trust for America’s Health and Well Being Trust. Our nation has struggled to implement proven solutions on a wide scale and in a sustained way that is sufficient to mitigate these problems.
The Impact of COVID-19
COVID-19 has irrevocably changed the face of the nation and unmasked pervasive systems failure and racial inequity, as Black and Hispanic adults in the U.S. are nearly 3 times more likely than white, non-Hispanic adults to die from the virus. Health inequities existed before the COVID-19 outbreak; current projections show they are worsening, particularly for communities of color, and will continue on this trajectory after the pandemic if no actions are taken to change their course.
Take, for example, a recent analysis from Well Being Trust and the Robert Graham Center on the pandemic’s impact on deaths from alcohol, drug abuse, and suicide. Deaths of despair have doubled over the past few decades, and rates are soaring further amid the COVID-19 pandemic. And the physical health disparities are being mirrored in mental health disparities.
Multiple factors affecting mental well-being are at work in the pandemic: unprecedented economic failure and massive unemployment; social dislocation and isolation; uncertainty caused by the sudden emergence of a contagious virus and widespread disinformation and misinformation; and recognition that it will take time for the vaccine to become universally available.
At the same time, because we are all suffering together during the pandemic, we’ve seen a glimmer of hope for those dealing with mental illness: more conversations, both online and off, about struggling with mental health and seeking help. The spread of COVID-19 and the necessity of keeping our distance from each other has meant Americans everywhere are experiencing degrees of loneliness, isolation, and anxiety. As a result, mental well-being has come to the forefront of our national conversation.
And yet, even though more Americans are talking more about the state of mental well-being, so far we have missed the chance to put our money where our mouths are and address the topic in federal stimulus relief bills. Limited resources were put into mental health, in fact, a fraction of what was put into the broader health care arena. And federal, state, and local governments have failed to do some of the most basic actions like place mental health experts in positions of leadership for our response.
With the fragmentation so pervasively codified through policy, COVID-19 has given all levels of government a chance to reassess their structures and challenge historically sacred tenets of delivery. Take, for example, the lifting and loosening of telehealth restrictions that has allowed more clinicians to see patients through virtual visits at the patient’s convenience. This notion of bringing care to the person is a strong one that should be supported through policy change, even after the pandemic is over.
To heal the nation, we need to take bold, concerted action. Leaders at all levels can apply the Framework for Excellence in Mental Health and Well-Being, a consensus approach to comprehensive change, featuring solutions spanning the workplace, the community at large, and the health, judicial, and education systems. We need investment in mental health now so local communities can play an essential role by promoting communitywide well-being.
A Clear Vision
Healing the nation requires a clear vision for what well-being looks like. It requires collective, coordinated action by community leaders to make robust, lifesaving, and resilience-building improvements. By addressing coverage, care, and community change all at once, we can assure well-being for all.
*Coverage
Access to affordable and comprehensive health insurance is a right. Yet, insurance providers’ coverage for mental health services often leaves consumers with high out-of-pocket costs or denies them treatments critical to their recovery and well-being. About 4 in 10 people in the U.S. (42%) said they could not seek mental health care in 2018 because they lacked insurance coverage.
To establish a standard of whole-person care — tending to the mind, body, and spirit — states can hold insurance companies accountable for covering a wide range of mental health and addiction services before deductibles and without referrals. Expanded access to medication, emergency overdose products, and treatments — as well as evidence-based treatment and recovery support services — will create a full-coverage health care system in which people can get the mental health and addiction care they need.
California’s new mental health and substance use disorder coverage law, SB 855, exemplifies state-level policy change that increases access to care by enforcing mental health parity with coverage for physical health. Signed into law in September 2020, the legislation requires insurers to adhere to a uniform definition of “medically necessary” determined by health professionals. They must cover treatment for mental health and addiction disorders according to that definition, just as they cover treatment for physical ailments.
* Care
Health care systems can improve the health and well-being of the populations they serve by aligning their institutional priorities with community needs. This is known as the “anchor institution” approach. Leveraging their purchasing and hiring power — as well as their hefty investment portfolios — to enact change, health care systems can catalyze long-term well-being and equity in the community.
To do so, hospitals must contribute to an environment that promotes flourishing. In support of Well Being Trust’s (WBT) goal to save 100,000 lives from deaths of despair and dramatically increase healthy life years in the next 10 years, the Institute for Healthcare Improvement developed a set of recommendations to leverage the role of health care systems to impact the health and well-being of the populations they serve within their walls and across their communities.
Under these guidelines, health care systems must focus on prevention and recovery as well as acute care. They must also work to increase access to care in as many places as possible, including homes, schools, workplaces, and jails and prisons. Providing care throughout the community, rather than primarily at hospitals and clinics, can help break down structural barriers that often prevent marginalized individuals from getting necessary care, paving the path to better health outcomes and long-term well-being for all.
Equally important is for health care systems to prioritize the mental and emotional well-being of their caregivers, including first responders at all levels — from doctors and nurses to cleaners and transportation professionals, all of whom endure risk and stress. Health system staff and medical professionals cannot give patients quality care if they are suffering themselves.
* Community
We vitally need a comprehensive approach to mental health and substance misuse at all levels of government. But local leaders need not — and cannot — wait for federal or state direction to pragmatically address mental, emotional, and spiritual well-being in bipartisan ways.
Local leaders know their communities, the places where they live. They can make changes in practice, policies and investments to create the vital conditions for mental health and well-being. The de Beaumont Foundation and Well Being Trust released a critical action guide for local leaders that includes more than 60 evidence-based policies, practices, and programs that can prevent further loss of life and livelihood from the nation’s growing mental health crisis.
The action steps are practical, many are low-cost or revenue-neutral, and address actions we need now and through long-term recovery from COVID-19. While the following steps are not traditionally considered mental health actions, they are essential to mental health equity and well-being for all:
- Provide incentives to create safe, affordable housing. Having a safe, stable place to call home is fundamental to leading a productive and fulfilling life. Community leaders can encourage affordable housing development in a number of ways, including dedicated funding streams for public-private partnerships, tax breaks and density bonuses — a financial incentive for building more units — for developers.
- Ensure access to green space for all. Similarly, leaders must prioritize public green space in community development. Establishing green space in communities can provide residents with the opportunity to develop social bonds and foster a sense of togetherness, which is critical for mental well-being.
- Cultivate a community-centered workforce. Leaders can cast a wide net to support mental health needs by leveraging community networks. This means coordinating a system of support that involves everyone from spiritual and faith leaders to teachers and community health workers. In a culture of trust and care, people can seek help wherever they are most comfortable in the community, expanding pathways to well-being and reducing the pressure and stress experienced by frontline providers.
Community partnerships that aim to improve well-being in a comprehensive, integrated way across sectors and siloes embody the spirit of the Framework. In Orange County, California, BeWell OC is a cross-sector initiative that works with public, private, academic, faith, and other institutions to ensure the best possible care for those with mental health and substance use disorders. The intentionally coordinated system involves six steps that engage the entire community: reducing stigma around mental health and addiction; increasing prevention and early intervention services; closing treatment gaps and improving access; strengthening crisis response support systems; establishing community wellness hubs for those seeking support; and aligning partners, policies, and programs to make sure there are no gaps in the system.
This cross-sector approach overcomes barriers to providing care for those experiencing mental health and substance use disorders that exist in traditional health care models, such as financial strains and lack of comprehensive health insurance.
Creating Conditions for Flourishing
The COVID-19 pandemic has made clear that we can no longer ignore the role that emotional well-being plays in economic and civic well-being — and in our chances to thrive in our communities and as a nation.
If the United States is going to continue to succeed in its glorious experiment in democracy, we are going to have to heal ourselves and our families, as well as our communities. The problem — and the solution — goes far deeper than the distracting superficial divisions between political parties. The pain that is being felt across this nation can be addressed in our communities, as we are seeing in reports such as Thriving Together. To go from a few bright spots to nationwide change, we must find common ground and build the political will to act together, rooted in the premise that whatever may divide us, that which connects us is greater still.
This is a call to action to local elected leaders and city agencies, nonprofits and philanthropy, business and health care executives, the faith community, media, and grassroots organizers: Embrace an integrated, systemic approach to creating the community conditions for social, emotional, and spiritual well-being. Our lives and nation depend on it.
Tyler Norris is CEO of Well Being Trust, and Benjamin F. Miller is chief strategy officer of Well Being Trust.



